Artificial Lung Technology Keeps Patient Alive Until Transplant
By Science Correspondent
Humans cannot survive without lungs — yet one patient did, for 48 hours.
In research published on 29 January in the Cell Press journal Med, surgeons revealed how they removed a patient’s severely infected lungs and used a temporary artificial lung system to keep him alive until donor lungs became available.
The case highlights how this method could act as a crucial bridge to lung transplantation.
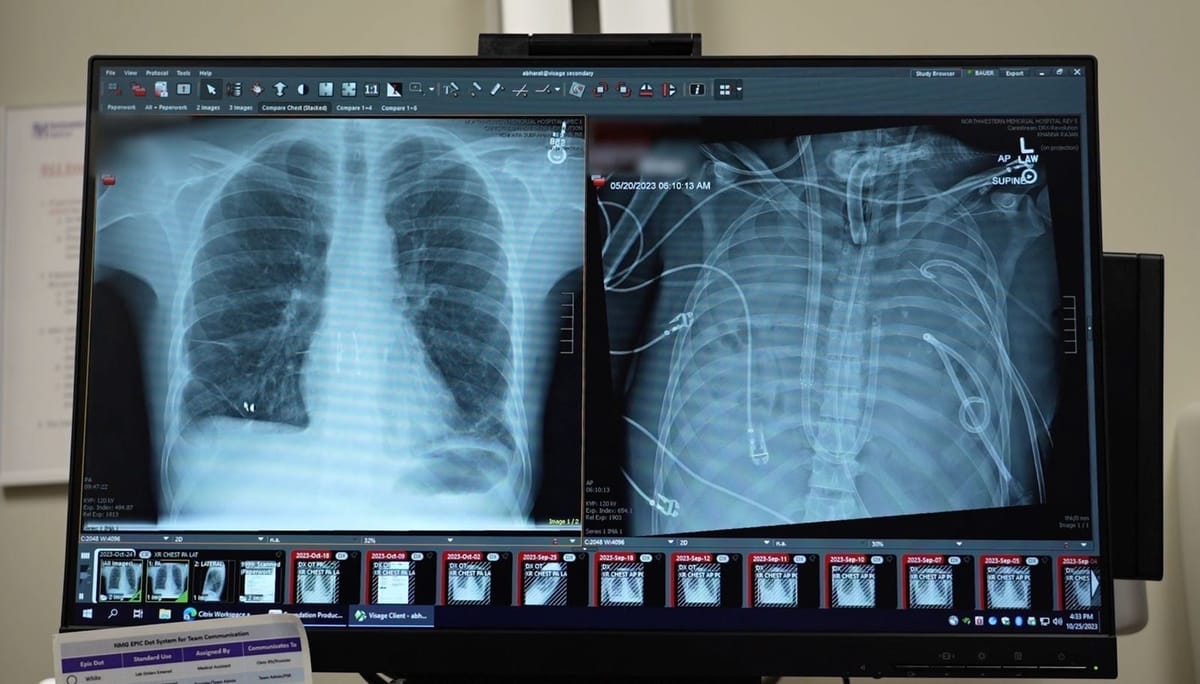
The patient, treated by a team led by thoracic surgeon Ankit Bharat at Northwestern University, was critically ill when he arrived at hospital. His heart stopped shortly after admission, and doctors were forced to perform CPR.
“When an infection becomes so aggressive that the lungs begin to disintegrate, the damage cannot be reversed,” Bharat explains. “That is usually when patients do not survive.”
The 33-year-old man developed acute respiratory distress syndrome (ARDS), a life-threatening condition caused by widespread inflammation and infection in the lungs.

Initially triggered by influenza, his condition worsened after he developed bacterial pneumonia. Soon, his lungs, heart, and kidneys began to fail, leaving a double lung transplant as his only chance of survival.
However, his lungs were not only beyond repair — they were also continuing to spread infection.
Despite this, his body was too unstable to immediately receive donor lungs and needed time to recover.
“The heart and lungs work as a single system,” says Bharat. “Without lungs, the challenge is keeping the rest of the body functioning.”
To overcome this, the surgical team created an artificial lung system that temporarily took over the lungs’ role. The system oxygenated the blood, removed carbon dioxide, and maintained stable circulation, allowing the patient to survive without lungs at all.
After the diseased lungs were removed, the patient’s condition began to improve.
His blood pressure stabilised, organ function recovered, and the infection reduced. Two days later, donor lungs became available, and surgeons successfully carried out a double lung transplant. More than two years on, the patient has returned to normal daily life with healthy lung function.
Traditionally, lung transplants are performed on patients with long-term conditions such as cystic fibrosis or interstitial lung disease. Severe ARDS, however, is often treated with the expectation that the lungs will eventually heal.
Analysis of the removed lungs told a different story. Molecular testing revealed extensive scarring and immune system damage, confirming that recovery was impossible.
“For the first time, we have biological evidence showing that some patients will not survive without a double lung transplant,” Bharat says.
While the technique is currently limited to specialist centres with advanced resources, Bharat hopes it will eventually be developed into more widely available technology.
“Too many young patients die because transplantation is never considered,” he says. “For severe lung damage caused by infections or viruses, even in acute cases, a lung transplant can save lives.”
READ PAPER HERE - Med, Yan, et al., “Bridge to transplant using a flow-adaptive extracorporeal total artificial lung system following bilateral pneumonectomy” https://www.cell.com/med/fulltext/S2666-6340(25)00412-X





